Understanding Ulcerative Colitis: Symptoms, Treatments, and Diet
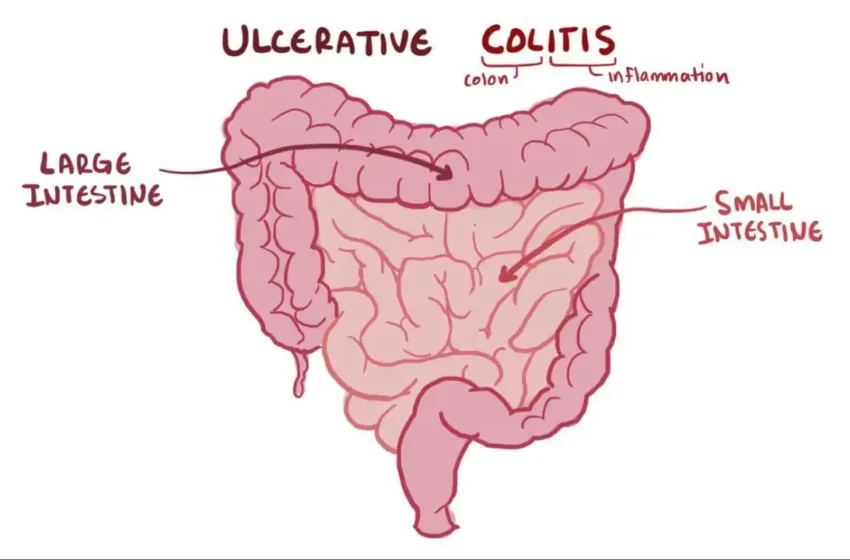
What Is Ulcerative Colitis?
Ulcerative colitis is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. Unlike Crohn’s disease, which can impact any part of the digestive tract, ulcerative colitis is limited to the large intestine. The condition causes inflammation and ulcers in the lining of the colon, leading to discomfort, pain, and digestive issues.
While the exact ulcerative colitis causes remain unclear, experts believe it results from an overactive immune response, genetic predisposition, and environmental factors. It is not contagious, but it can significantly impact quality of life if not managed properly.
Ulcerative Colitis Symptoms
The symptoms of ulcerative colitis vary depending on the severity of inflammation. Common signs include:
-
Persistent diarrhea, often with blood or mucus
-
Abdominal pain and cramping
-
Urgent bowel movements
-
Fatigue and weight loss
-
Loss of appetite
-
Fever in severe cases
Some people may also experience joint pain, skin rashes, or eye inflammation due to systemic inflammation.
Ulcerative Colitis Symptoms in Females
While many symptoms are similar across genders, ulcerative colitis symptoms in females may sometimes be mistaken for gynecological issues due to overlapping pelvic discomfort. Hormonal fluctuations can also influence flare-ups, particularly during menstruation, pregnancy, or menopause.
Ulcerative Colitis vs. Crohn’s Disease
A common question is the difference between Crohn’s vs. ulcerative colitis. Both are types of IBD, but they affect the digestive system differently:
-
Ulcerative colitis only involves the colon and rectum, with continuous inflammation.
-
Crohn’s disease can affect any part of the digestive tract, from mouth to anus, with patchy inflammation.
Understanding this distinction helps in accurate diagnosis and treatment.
Ulcerative Colitis Causes and Risk Factors
While the exact what causes ulcerative colitis is unknown, several factors contribute:
-
Genetics – A family history of IBD increases risk.
-
Immune system dysfunction – The body mistakenly attacks healthy colon cells.
-
Environmental triggers – Diet, stress, and infections may play a role.
Smoking, interestingly, has a complex relationship—while it worsens Crohn’s disease, it may slightly reduce ulcerative colitis risk, though smoking is never recommended due to other health risks.
Ulcerative Colitis Treatments
There is no cure for ulcerative colitis, but effective ulcerative colitis treatments can manage symptoms and induce remission. Treatment options include:
Ulcerative Colitis Medication
-
Anti-inflammatory drugs (aminosalicylates) reduce colon inflammation.
-
Corticosteroids help control severe flare-ups but aren’t for long-term use.
-
Immunosuppressants prevent the immune system from attacking the colon.
-
Biologics target specific proteins causing inflammation.
Ulcerative Colitis Surgery
In severe cases, ulcerative colitis surgery may be necessary. A colectomy (removal of the colon) can eliminate the disease but requires lifestyle adjustments, such as using an ostomy bag or undergoing a procedure to create an internal pouch.
Ulcerative Colitis Diet: What to Eat and Avoid
Diet plays a crucial role in managing ulcerative colitis. While triggers vary by person, some general guidelines help:
Best Foods for Ulcerative Colitis
-
Low-fiber foods (white rice, bananas, oatmeal)
-
Lean proteins (chicken, fish, eggs)
-
Cooked vegetables (carrots, squash)
-
Probiotic-rich foods (yogurt, kefir)
Worst Foods for Ulcerative Colitis
Common triggers include:
-
High-fiber foods (nuts, seeds, raw veggies)
-
Dairy (if lactose intolerant)
-
Spicy foods
-
Alcohol and caffeine
A 7-day meal plan for ulcerative colitis can help structure eating habits during flare-ups and remission.
Living with Ulcerative Colitis
Managing ulcerative colitis requires a combination of medication, diet, and lifestyle adjustments. Stress management techniques like meditation and gentle exercise can also help reduce flare-ups.
Regular check-ups with a gastroenterologist ensure proper monitoring. The ulcerative colitis ICD 10 code (K51) is used for medical classification and insurance purposes.
Final Thoughts
While ulcerative colitis is a lifelong condition, proper treatment and lifestyle changes can lead to long periods of remission. If you experience persistent ulcerative colitis stool changes (bloody or frequent diarrhea), consult a doctor for an accurate diagnosis and personalized treatment for ulcerative colitis.
By understanding the ulcerative colitis symptoms, ulcerative colitis treatments, and dietary needs, individuals can take control of their health and improve their quality of life.